Knee Osteoarthritis – What is this and how can you treat it?
Knee Osteoarthritis affects many in the general population, usually people over the age of 40. There is a perception that this condition is not able to be effectively treated. Thankfully this is not usually the case.
What is Knee Osteoarthritis?
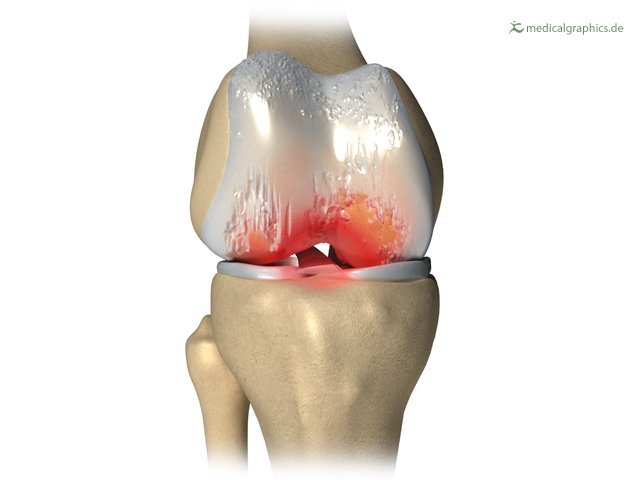
Osteoarthritis is a degenerative disease characterised by damage to joints over time and failure for them to repair and restore their natural state.
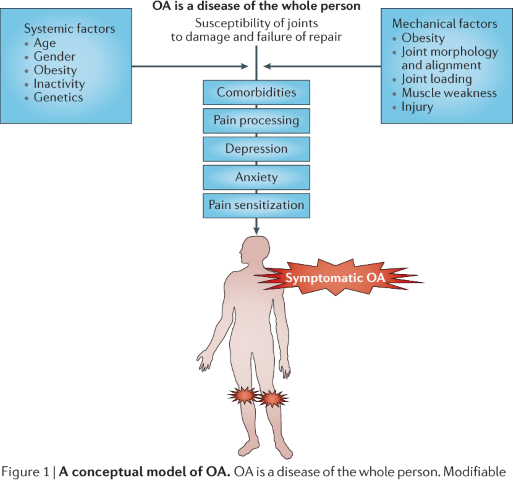
This condition involves much more than the simple structures of the knee. We understand this because the amount of structural changes to the knee, doesn’t correlate with the amount of pain you will experience.
Now-days researchers look at mechanical factors and also systemic factors.
Mechanical Factors for osteoarthritis include:
- Joint narrowing and bony growth
- Obesity
- Joint alignment
Systemic Factors for osteoarthritis include:
- Age
- Gender
- Obesity
- Genetics
All the above factors and more can influence the pain someone experiences with knee osteoarthritis. These factors are further influenced by the way an individual processes pain – their pain tolerance.
Below is a figure taken from a research paper titled ‘strategies for the prevention of knee osteoarthritis’.
Prevalence
The literature would suggest that approximately 13% of women and 10% of men are diagnosed with symptomatic knee osteoarthritis.
These numbers are generally made up of people over the age of 60, however there are younger people that struggle with knee osteoarthritis as well.
The proportion of people with degenerative changes on X-ray is much higher, however not all of these people have symptoms.
Symptoms of knee osteoarthritis
Symptoms of knee osteoarthritis follow a very simple pattern.
The knee will usually be stiff first thing in the morning, but it should warm up in less than 30 minutes. If it takes longer to warm up, this could indicate the presence of other diseases such as rheumatoid arthritis.
The knee is usually very stiff after sitting for a long
period of time and when you first stand you will probably notice some pain.
There should be tenderness along the inside or outside of the
knee, and the knee could look like it buckles in or bows – depending on which
side of the joint is degenerating.
The knee could be painful after long periods of walking,
jogging, squatting or stairs.
If the degenerative changes are getting worse, people can experience locking and giving way of the knees. This is a sign that you may need surgical input. For other reasons your knee could give way please read our blog on ‘7 reasons why your knee gives way’
Keep in mind that knee osteoarthritis is a continuum. This
means some people could have very mild symptoms, whilst other people could have
severe symptoms.
Imaging for knee osteoarthritis
As previously mentioned, knee osteoarthritis affects many
structures within the joint. You will find changes to bone, meniscus, cartilage
and joint capsule.
The Kellgren-Lawrence scale is the most commonly used for grading the severity of knee osteoarthritis.
This scale takes into account factors such as:
- Joint space narrowing
- Bony spurs – also called osteophytes
- Increased density of the bone around the joint line (sclerosis)
- Bony deformity
It is important to note that these changes are judged by a
weight-bearing X-ray. This means you are standing as the X-ray is taken, which
emphasizes any joint space narrowing.
Do I need an X-ray?
It is now common practise to have knee osteoarthritis
diagnosed without any imaging. This is due to the relative ease of clinical
diagnoses.
X-rays can be used to confirm a clinician’s suspicion, but
rarely adds anything valuable to the examination. X-rays are harmful to the
patient as they can look very different to how the patient feels and expose the
patient to radiation.
Remember that 50% of patients don’t have symptoms, even if the imaging reports reveal changes to the bone structure.
Do I need
an MRI?
There is often no need to have an MRI. MRI’s are very expensive and will only be used if there is suspicion of something more sinister mimicking knee osteoarthritis.
Risk factors for
Knee Osteoarthritis
The risk factors for knee osteoarthritis are sensible. Some
of the risk factors include:
- Old age – as we age, we begin to wear out
- Obesity – there is a link between increased
adipose tissue and knee pain. - Repetitive tasks which load the knee such as
squatting or kneeling - Trauma to the knee – including old injuries
which change the joint mechanics
The link between obesity and knee pain
Obesity can affect knee osteoarthritis in more ways than simply the load through the knee. Studies have shown that people with hand and shoulder arthritis do better when they lose weight. This can’t be explained through load, as the hand and shoulder aren’t weight bearing joints.
For further explanation on the hidden link between obesity and knee pain read our article on ‘weight loss does more for knee pain than you think’.
Treatment for
Knee Osteoarthritis
Treatment for knee osteoarthritis need to be tailored to the individual. This is where online physiotherapy is set up for success.
With an online physiotherapist you can journey with through
the week, asking questions when needed. Rehabilitation via videoconference is
very plausible as manual techniques are not needed for the treatment of knee
osteoarthritis.
There are two areas that need to be targeted:
- Weight loss
- Home Remedies
- Strength, aerobic and neuromuscular training
Weight loss
Targeting weight for knee osteoarthritis is incredibly
important as it will help to reduce the inflammation carried through the blood
stream. Weight loss has other benefits including increased energy levels which
will help to keep the cycle of exercising going.
Weight loss is dependent on your level of physical activity and your dietary habits. If you can modify both your diet and your physical activity, weight loss will be a natural consequence.
Although dietary input is not our field of expertise it is
wise to try small meals sizes and eat 4-5 meals per day. Start with your
biggest meal in the morning and eat whole foods.
Physical activity does happen to be our area of expertise so
let’s elaborate:
Home Remedies and supplements
There are many home remedies suggested for the treatment of knee osteoarthritis. These remedies may lack robust clinical trials, however patients can find them to work very well.
Among many supplements on the market, some that come up often are tumeric and fish oil. These supplements can help in reducing inflammation and maintaining the joint fluid.
Strength, aerobic and neuromuscular training
Although physical activity can be as simple as walking the
dog, there needs to be a level of intentionality for people suffering with knee
osteoarthritis.
A good exercise regime will be split into the three
components listed above.
Strength training
Strength training involves mainly strengthening your
quadriceps muscle. We have a video of an exercise that is easy to perform in
any home environment just below:
Aerobic training
Aerobic training can involve any exercise that really gets
your heart pumping. For some this may be a walk, others might enjoy swimming
and still others could box. When deciding what aerobic exercise you should
perform, take into account what you like.
‘you will be consistent when you’re content with the exercise’
Neuromuscular exercise
Neuromuscular training involves working on movement patterns
and correct muscle activation. These are very specific exercises meant to help
switch on the right muscles for improved motor control during tasks.
We have a quick 15 second video of a neuromuscular exercise
aimed as firing up your bottom muscles. With this exercise you should feel a
pull in your outer bottom area of the leg you are leaning towards. The idea is
to lean all your weight onto that leg and hitch your hip so that it stays level
as you move.
Surgery for Knee Osteoarthritis
There is now only one option for advanced knee
osteoarthritis which is a total knee replacement.
In the past the surgical options also included a knee
arthroscopy where they went in and shaved the cartilage back to make it as
smooth as possible.
Now, research has proven that knee arthroscopies for knee
osteoarthritis have little to no effect. Some surgeons will still offer this
procedure, and very few people may benefit from it, however this is not
recommended practise these days.
Total knee replacement
A total knee replacement involves cutting back the bone on
either side of the knee joint and replacing it with two metal plates that rub
against one another. This surgery usually results in reduced pain and improved
function.
Surgeons will usually offer this surgery to people over 50 years old who have failed conservative treatment (treatment like physiotherapy and pain medication). People with symptoms like giving way of the knee are more likely to benefit from this surgery as well.
High tibial osteotomy
This surgery can be offered to younger patients who only
have osteoarthritis on one side of the knee. The surgery involves cutting a
wedge out of the shin bone to re-align the knee joint and put more weight on
the side that isn’t affect by the osteoarthritis.
The bottom line:
Knee osteoarthritis is a lifelong disease with a varied progression. The main-stage treatment is physiotherapy which involved weight lose and strength/neuromuscular training. As a last resort, surgery can be considered, although a total knee replacement is the only reliable surgery for people with advanced osteoarthritis.
References:
Ewa M. Roos, & Nigel K. Arden. (2015). Strategies for the prevention of knee osteoarthritis. Nature Reviews Rheumatology, 12(2), 92–101. https://doi.org/10.1038/nrrheum.2015.135
Heidari B. (2011). Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian journal of internal medicine, 2(2), 205–212.

